

•The consumption of a more cariogenic, soft, and pureed diet by children with disabilities (especially the ones with mental retardation, and generalized hypotonia) meaning food retention in the mouth for a long time prior to swallowing.
Teeth grinding (bruxism)
Teeth grinding (bruxism) is the involuntary clenching or grinding of the teeth. It generally happens during sleep, but some people experience it when they are awake.
Complications of teeth grinding
Teeth grinding can cause a range of oral health problems, which may include:
cracked tooth enamel
excessive wear and tear on the teeth
broken teeth or restorations
strain on the joints and soft tissue of the jaw joint
enlargement of the jaw muscles (rare).
Signs and symptoms
The signs and symptoms of teeth grinding include:
grinding sounds while the person is asleep
headache, jaw joint or ear pain
aching (or ‘dancing’) teeth – particularly upon waking
aching or stiffness of the face and temples upon waking
aching or stiffness in the jaws while chewing – particularly during breakfast
clenching the jaw when angry, anxious or concentrating
sensitive teeth
cracked or chipped tooth enamel
tooth indentations on the tongue
raised tissue on the cheek caused by cheek biting
wobbly teeth.
Causes
Some of the factors that may trigger grinding include:
emotional stress, such as anger or anxiety
mental concentration
physical effort or stress, such as illness, nutritional deficiency or dehydration
Incorrect tooth alignment
Drug misuse (particularly amphetamines)
Eruption of teeth (babies and children)
What you should do?
If you think you may be grinding your teeth, see your oral health professional as soon as possible. They will examine your teeth and may take x-rays to check the severity of the problem and the damage done to teeth and bone. They might also suggest some therapy to assist in removal or reduction in the habit.
Teeth grinding in children
Many children grind their teeth at some stage. Some children clench their jaws quite firmly. Others grind so hard that it makes a noise.
Children will not usually be woken up by the sound of their own teeth grinding – but other people in the room might be!
In most cases, children who grind their teeth don’t cause any damage to their teeth. In only a few very extreme cases, where the grinding is very regular, is it likely that your child could cause damage to teeth.
If you’re concerned, talk to an oral health professional.

Knocked out or broken teeth
If permanent teeth are knocked out, there is an excellent chance that they will survive if they are immediately placed back in the tooth socket and dental health advice is sought straight away. Every minute the tooth is out of the socket, the less chance it has of surviving.
Adult tooth knocked out – what should I do?
If the knocked out tooth is dirty, gently rinse it with milk without touching the root and follow the steps below. Do not scrub.
Stay calm and act quickly.
Locate the tooth and hold it by the crown (smooth white part).
If the root has dirt on it, gently rinse the tooth in milk or saline solution such as contact lens solution for a few seconds only – do not use water or scrub.
If the person is conscious, hold the cleaned tooth by the crown and replace it into its socket using light pressure.
Hold the tooth in place by getting the person to gently bite on a handkerchief.
Seek immediate advice or treatment from an oral health professional
If you can’t replace the tooth:
Do not let it become dry and do not use tap water.
Place the tooth in milk or saliva (preferably the patient’s).
Seal it in plastic wrap.
Seek immediate advice or treatment from an oral health professional.
Knocked out baby tooth – what should you do?
Do not try to put a baby tooth back in its socket because:
It may fuse to the socket, which leads to difficulties when it is time for the tooth to be shed.
It may damage the permanent tooth underneath the socket.
Broken or fractured tooth – What should you do?
Cracked or fractured teeth may or may not be painful. It is recommended that you see an oral health professional, as early recognition can improve the survival of the damaged tooth.
If the tooth fragment is broken and is intact, store it in milk or saliva (preferably the patient’s).
Seal it in plastic wrap.
See an oral health professional as soon as possible.

TOOTH EXTRACTIONS
You and our doctors may determine that you need a tooth extraction for any number of reasons. Some teeth are extracted because they are severely decayed; others may have advanced periodontal disease, or have broken in a way that cannot be repaired. Other teeth may need removal because they are poorly positioned in the mouth (such as impacted teeth), or in preparation for orthodontic treatment.
The removal of a single tooth can lead to problems related to your chewing ability, problems with your jaw joint, and shifting teeth, which can have a major impact on your dental health.
To avoid these complications, in most cases, Our doctors will discuss alternatives to extractions as well as replacement of the extracted tooth.
The Extraction Process
At the time of extraction the doctor will need to numb your tooth, jaw bone and gums that surround the area with a local anesthetic.
During the extraction process you will feel a lot of pressure. This is from the process of firmly rocking the tooth in order to widen the socket for removal.
You feel the pressure without pain as the anesthetic has numbed the nerves stopping the transference of pain, yet the nerves that transmit pressure are not profoundly affected.
If you do feel pain at any time during the extraction please let us know right away.
Sectioning a Tooth
Some teeth require sectioning. This is a very common procedure done when a tooth is so firmly anchored in its socket or the root is curved and the socket can’t expand enough to remove it. The doctor simply cuts the tooth into sections then removes each section one at a time.
After Tooth Extraction
After tooth extraction, it’s important for a blood clot to form to stop the bleeding and begin the healing process. Bite on a gauze pad for 30-45 minutes immediately after the appointment. If the bleeding or oozing still persists, place another gauze pad and bite firmly for another 30 minutes. You may have to do this several times to staunch the flow of blood.
After the blood clot forms it is important to not disturb or dislodge the clot. Do not rinse vigorously, suck on straws, smoke, drink alcohol or brush teeth next to the extraction site for 72 hours. These activities may dislodge or dissolve the clot and hinder the healing process. Limit vigorous exercise for the next 24 hours, as this increases blood pressure and may cause more bleeding from the extraction site.
After the tooth is extracted you may feel some pain and experience some swelling. An ice pack or an unopened bag of frozen peas or corn applied to the area will keep swelling to a minimum. Take pain medications as prescribed. The swelling usually subsides after 48 hours.
Use pain medication as directed. Call our office if the medication doesn’t seem to be working. If antibiotics are prescribed, continue to take them for the indicated length of time even if signs and symptoms of infection are gone. Drink lots of fluids and eat nutritious, soft food on the day of the extraction. You can eat normally as soon as you are comfortable.
It is important to resume your normal dental routine after 24 hours. This should include brushing and flossing your teeth at least once a day. This will speed healing and help keep your mouth fresh and clean.
After a few days you should feel fine and can resume your normal activities. If you have heavy bleeding, severe pain, continued swelling for 2-3 days, or a reaction to the medication, call our office immediately.
WISDOM TEETH REMOVAL
Oral Examination
With an oral examination and x-rays of the mouth, our doctor can evaluate the position of the wisdom teeth and predict if there are present or future potential problems. Studies have shown that early evaluation and treatment result in a superior outcome for the patient. Patients are generally first evaluated in the mid-teenage years by their dentist, orthodontist, or by an oral and maxillofacial surgeon.
All outpatient surgery is performed under appropriate anesthesia to maximize patient comfort. Our doctors are trained, licensed, and highly experienced in providing various types of anesthesia for patients.
Why Should I Have My Wisdom Teeth Removed?
If you do not have enough room in your mouth for your third molars to fully erupt, a number of problems can happen. Impacted wisdom teeth should be removed before their root structure is fully developed. In some patients it is as early as 12 or 13, and in others it may not be until the early twenties. Problems tend to occur with increasing frequency after the age of 30. Some of the possible problems related to not removing your wisdom teeth include:
Infection:
The most frequent clinical problem we see is pericoronitis, (a localized gum infection). Without enough room for total eruption, the gum tissue around the wisdom tooth can become irritated and infected, resulting in recurrent pain, swelling, and problems with chewing and/or swallowing.
Cyst Formation:
Non-infectious diseases may also arise in association with an impacted wisdom tooth. Cysts are fluid-filled “balloons” inside the jaw bone that develop as a result of impacted teeth and slowly expand destroying adjacent jaw bone and occasionally teeth. They can be very difficult to treat if your wisdom teeth are not removed in your teenage years. Although rare, tumors can be associated with the delayed removal of wisdom teeth.
Possible Crowding:
Impacted wisdom teeth may contribute to crowding of your teeth. This is most noticeable with the front teeth, primarily the lower front teeth and is most commonly seen after a patient has had braces. There are a number of factors that cause teeth to crowd after braces or in early adulthood. Retained, impacted wisdom teeth may be a contributing factor. Unless you have an active problem when you see your dentist, the reason for removal is primarily to prevent long-term damage to your teeth, gums and jaw bone.
Damage to Adjacent Teeth:
If there is inadequate room to clean around the wisdom tooth, the tooth directly in front, the second molar, can be adversely affected resulting in gum disease, bone loss around the tooth, and/or decay.
What If I Don’t Have My Wisdom Teeth Removed As A Teenager Or Young Adult?
As wisdom teeth develop, the roots become longer and the jaw bone more dense.When it is necessary to remove impacted wisdom teeth in your thirties, forties or beyond, the post-operative course can be prolonged and there is a higher complication rate. Treating these complications is often more difficult and less predictable than with a younger patient. Healing may be slower and the chance of infection can be increased. If your impacted wisdom teeth are not removed in your teenage years or early in your twenties and they are completely impacted in bone, it may be advisable to wait until a localized problem (such as cyst formation or localized gum disease and bone loss) develops. In general, you will heal faster, more predictably and have fewer complications if treated in your teens or early twenties.
What Happens On The Day Wisdom Teeth Are Removed?
Most people prefer to be unaware of the experience when they have their wisdom teeth removed and usually decide to be sedated. You will be provided with appropriate anesthesia options at your consultation. All outpatient surgery is performed under appropriate anesthesia to maximize your comfort. Our office staff has the training, licensing, and experience to provide the various types of anesthesia. These services are provided in an environment of optimum safety, utilizing modern monitoring equipment and a well trained experienced staff. The Surgical Care Team, the office facilities, and the doctors are inspected on behalf of the Board of Dental Examiners on a regular basis.
On the day of your procedure, you will take medications to help minimize post-operative pain and swelling. We ask that a parent or responsible adult accompanies you to the office and plans to stay with you the rest of the day. The procedure will take about 30 to 60 minutes and you will probably be in the office for 90 minutes. Recent advances in medicine and technology allow patients to undergo wisdom tooth removal in a manner, which promotes rapid healing and minimal post-operative discomfort. State of the art sterilization and infection control techniques are used at all times.
On the morning or afternoon of your surgery, it is essential that you have nothing to eat or drink (excluding prescription medications with a sip of water) for at least 6 hours (preferably longer). This does not mean you should try to fit in one “last meal” exactly six hours before your surgery. Having anything in your stomach can increase the risk for serious anesthetic complications, including nausea and vomiting. Your procedure will be rescheduled if you have not heeded these guidelines. We may provide you with a prescription for pain medication at your consultation appointment, which for your convenience, can be filled in advance. When you are seated in the surgical room, we will make every effort to make you as comfortable as possible. If you are going to be sedated, we usually will place an IV in your left arm. This is a quick and nearly painless procedure that ensures optimal delivery of your medication. Local anesthesia is given to you afterwards to ensure comfort, and allow adequate time to travel home and rest. You will be sleepy for a significant portion of the day.

How to brush your teeth
Daily brushing and cleaning between your teeth is important because it removes plaque. If the plaque isn’t removed, it builds up and can cause tooth decay and gum disease. You should brush your teeth at least twice a day and toothbrushes should be replaced every 3-4 months, or when the bristles get worn or frayed.
The five steps below show you how to brush your teeth correctly.
1.Brush in the morning and at night before going to bed.
2.Use a pea-sized amount of toothpaste on a soft toothbrush.
3.Brush teeth and along the gum using a gentle circular motion. Start with the outside surfaces.
4.Repeat on the inside surfaces.
5.Use a light back and forth motion on the chewing surfaces. Spit out toothpaste, but don’t rinse with water.
How to brush your child’s teeth (0-6 years)
Caring for your baby’s teeth and gums
Under 18 months
If your baby doesn’t like having their teeth brushed, you could try to make brushing more fun by singing songs or letting your baby play with a toy. Even a quick attempt at brushing is better than nothing, so your baby starts to learn that brushing is a normal part of their daily routine.
Starting a routine early gives your baby the best chance for healthy teeth.
When do I start caring for my baby’s teeth?
As soon as your baby’s first tooth appears, gently brush using a small, soft toothbrush. Or you can wipe with a damp, clean face washer instead.
Brush or wipe teeth with water until your baby is 18 months old.
Even before teeth appear, you can wipe baby’s gums using a damp, clean face washer. This can help get your baby ready for toothbrushing.
When do I start using toothpaste?
When your baby is 18 months old brush with children’s low fluoride toothpaste.
How often do I brush my baby’s teeth?
Brush in the morning and at night before bed.
How to brush your child’s teeth?
18 months to 6 years
Tips:
Choose a position where you can see your child’s teeth. Try different positions that work for you and your child.
As your child becomes more independent let them have a go at brushing their teeth. Finish by brushing them yourself.
Children need help to brush teeth up to at least 8 years of age.
Brush in the morning and at night before bed.
Use a pea-sized amount of low fluoride children’s toothpaste on a soft toothbrush
Brush the outside surfaces using gentle circles.
Next, brush the inside surfaces using gentle circles.
Use a light back and forth motion on the chewing surfaces, top and bottom.
Ask your child to spit out the toothpaste and not rinse with water.
Not rinsing the fluoride toothpaste away helps to protect teeth.
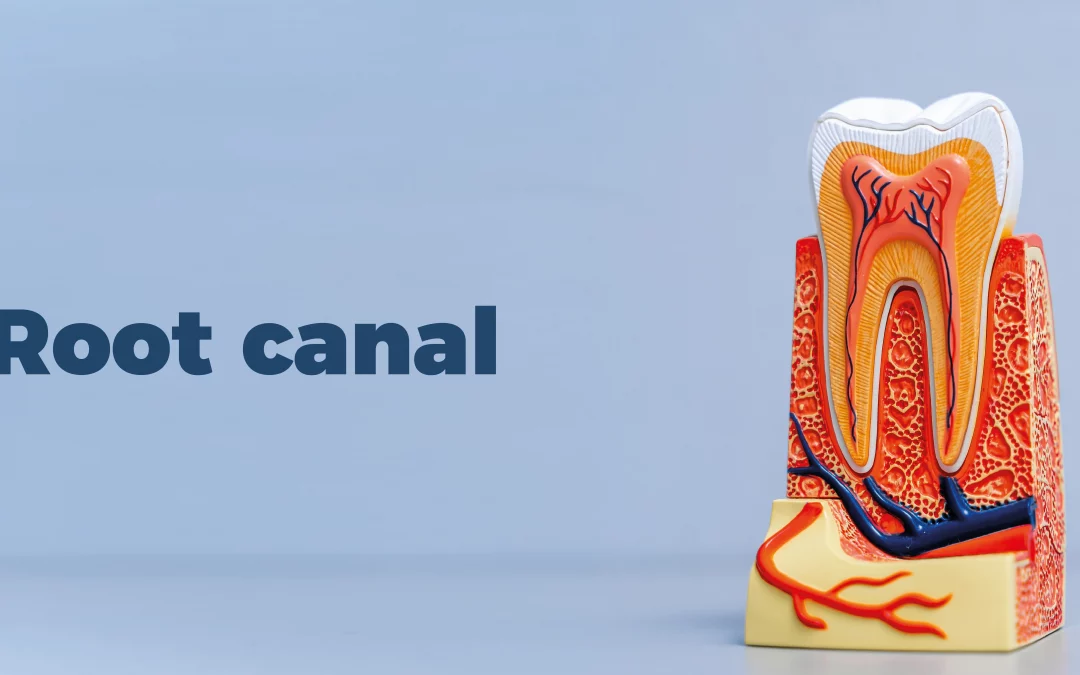
ROOT CANAL
ROOT CANAL
What is a root canal?
A root canal is one of the most common dental procedures performed, well over 14 million every year. This simple treatment can save your natural teeth and prevent the need of dental implants or bridges.
At the center of your tooth is pulp. Pulp is a collection of blood vessels that helps to build the surrounding tooth. Infection of the pulp can be caused by trauma to the tooth, deep decay, cracks and chips, or repeated dental procedures. Symptoms of the infection can be identified as visible injury or swelling of the tooth, sensitivity to temperature or pain in the tooth and gums.
If you experience any of these symptoms, your dentist will most likely recommend non-surgical treatment to eliminate the diseased pulp. This injured pulp is removed and the root canal system is thoroughly cleaned and sealed. This therapy usually involves local anesthesia and may be completed in one or more visits depending on the treatment required. Success for this type of treatment occurs in about 90% of cases. If your tooth is not amenable to endodontic treatment or the chance of success is unfavorable, you will be informed at the time of consultation or when a complication becomes evident during or after treatment. We use local anesthesia to eliminate discomfort. In addition, we will provide nitrous oxide analgesia, if indicated. You will be able to drive home after your treatment, and you probably will be comfortable returning to your normal routine.
Root canal treatment
What is a root canal treatment?
Inside the tooth is a hollow centre containing ‘pulp’. Pulp is a sensitive tissue made up of blood vessels and nerves that provides oxygen, nutrients and feeling to the tooth.
The pulp is found all through the tooth and the space where the pulp sits in the root is called the root canal.
Root canal treatment is a dental procedure that replaces damaged or infected pulp in the tooth’s root canal, with a filling.
Why might I need a root canal treatment?
If you have damaged or infected pulp in one or more of the roots of your teeth, or an abscess has developed, you may need a root canal treatment. This damage or infection may have been caused by untreated dental decay, decay beneath a filling, tooth damage, tooth grinding (bruxism ) or gum disease.
Please note: Root canal treatment will not be offered if the tooth is loose or if only a small amount of tooth remains as the treatment is not likely to be successful in these cases.
What should I expect with root canal treatment?
This procedure may need to be completed over several visits.
The infected tooth.
The dental professional will make an opening in the top of the tooth.
The diseased pulp and bacteria are flushed out with disinfectant and the root canals are cleaned with special instruments.
The pulp chamber and root canals are filled and sealed.
The tooth opening is restored with a filling.
After a root canal treatment, a tooth becomes brittle. It can be strengthened (to stop it from splitting while eating) with a cap or ‘crown’.
What are the alternatives to a root canal treatment?
Remove the tooth – Removing the tooth will leave a gap that may need to be replaced by an artificial tooth.
Leave the tooth untreated – If left untreated an infection may occur and can spread to the jaw. Pus can build up and cause pain. Cysts may also develop and need further treatment.

